H. pylori Treatment: Why It Is Challenging
26 Aug, 2025
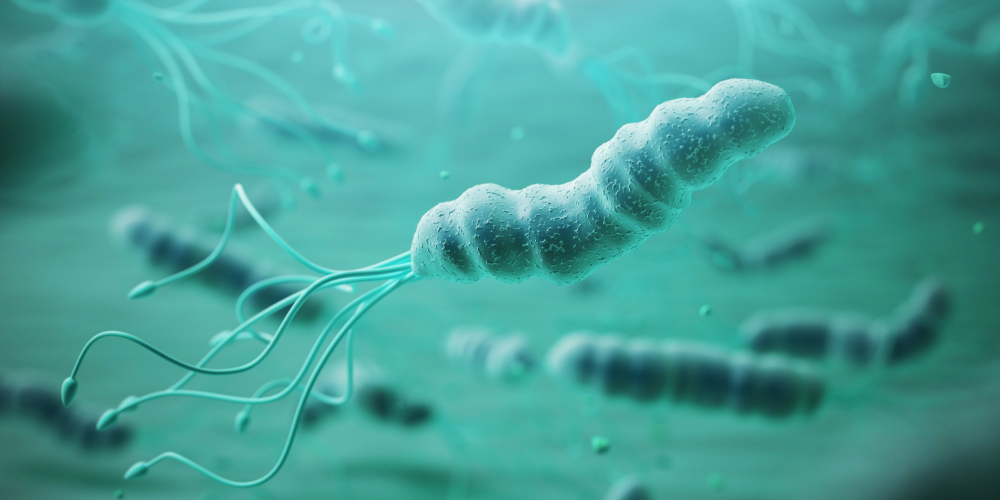
Helicobacter pylori, or H. pylori infection often causing gastritis, peptic ulcers, and sometimes more severe complications like stomach cancer. While many people carry H. pylori without symptoms, those who do experience symptoms can face digestive discomfort, nausea, and pain. The good news is that H. pylori is treatable, but the treatment process is not always straightforward.
H. pylori treatment has been an ongoing challenge in the medical field, due to a number of factors that make eradication difficult. These challenges, including antibiotic resistance, non-compliance with treatment, and other factors, make it harder to successfully treat this common infection.
The Challenges in Treating H.pylori
1. Antibiotic resistance
One of the primary reasons why pylori treatment is challenging is the growing issue of antibiotic resistance. Over the years, H. pylori have developed resistance to commonly used antibiotics like clarithromycin and metronidazole. Antibiotic resistance occurs when the bacteria mutate and adapt to withstand the effects of the drugs designed to kill them. This means that standard treatment regimens, which typically use a combination of antibiotics, may no longer be as effective.
Resistance reduces the likelihood of successful eradication and may require doctors to prescribe alternative antibiotics or use higher doses. In some cases, this may lead to prolonged treatment or the need for more aggressive therapy, such as quadruple therapy, which includes more medications to fight resistant strains.
2. Patient adherence to treatment
Successful treatment of pylori requires patients to adhere strictly to a regimen that often lasts 10-14 days. However, completing this course of therapy can be difficult for some patients. The medications may cause side effects like nausea, diarrhea, or a metallic taste in the mouth, leading some patients to stop the treatment prematurely. When patients do not complete the full course, it can lead to incomplete eradication of the bacteria, allowing it to come back or even develop resistance to the antibiotics.
Additionally, the complexity of the treatment regimen can deter patients from adhering to it. Triple therapy involves taking multiple pills at different times of the day, which can be overwhelming for some individuals. Ensuring patient education about the importance of completing the treatment is critical to achieving the desired outcomes.
3. Reinfection or recurrence
Even after a successful treatment course, there is a risk of reinfection or recurrence. Reinfection can occur if a person comes into contact with contaminated food, water, or individuals who carry the bacteria. Recurrence can also happen if the initial infection was not fully eradicated, which may be due to incomplete treatment or antibiotic resistance. Reinfection is more common in areas with poor sanitation and hygiene practices, making prevention efforts a crucial aspect of managing pylori.
4. Complexity of treatment
Treating H. pylori infection is not just about using the right antibiotics, it is about using them in combination with other medications. Proton pump inhibitors (PPIs) are typically prescribed alongside antibiotics to reduce stomach acid and help heal any damage caused by the infection. This combination therapy can be challenging to manage, and doctors must carefully choose the appropriate drugs for each patient based on their health, medical history, and the resistance profile of the bacteria.

Antibiotic Resistance and Its Impact on Treatment
Antibiotic resistance in H. pylori is a growing problem that affects treatment success. When the bacteria resist certain antibiotics, it can make standard treatments less effective. This can lead to longer treatments, the use of more expensive or potent drugs, or the need for more invasive options like quadruple therapy, which involves four medications instead of three.
The increasing resistance to clarithromycin, in particular, has prompted healthcare providers to rethink treatment strategies. In regions with high resistance rates, alternative antibiotic combinations may be needed, and more advanced diagnostic tests are used to tailor the treatment to the specific strain of H. pylori infecting the patient.

Adherence to Treatment and Patient Compliance
Patient adherence to treatment is essential for the success of H. pylori therapy. The complexity of the treatment regimen, combined with side effects, can lead to non-compliance. When patients do not follow the prescribed treatment correctly, it can result in the bacteria surviving and continuing to cause damage.
Strategies to improve adherence include simplifying the treatment regimen, offering medication combinations in single-dose forms, and providing clear instructions on how to take the medication. Educating patients about the importance of completing the full course of therapy, even if they start feeling better, is also crucial.
Alternative Treatment Approaches
For patients with antibiotic-resistant H. pylori strains or those who fail initial treatment, quadruple therapy may be recommended. This involves using a combination of:
- Two antibiotics (such as tetracycline and metronidazole)
- A proton pump inhibitor (PPI)
- Bismuth subsalicylate, which has antibacterial properties and helps protect the stomach lining
Quadruple therapy is often more effective for patients with resistant strains of H. pylori, though it is more intensive and may have more side effects. In some cases, doctors may also consider “sequential therapy,” where different antibiotics are given in a sequence over time to avoid resistance.
Co-medication of H. pylori therapy with saccharomyces boulardii helps to improve treatment outcome by:
- Protecting the gut microbiome during antibiotic treatment
- Improving patient tolerance & adherence by reducing side effects such as nausea and diarrhea
- Enhancing eradication success by supporting a balanced gut environment

MEGA Normagut supports gut health by preventing and treating antibiotic-associated diarrhea. This helps healthcare providers offer more effective treatment strategies and improve patient outcomes.
References:
Bagirova M, Allahverdiyev AM, Abamor ES, Aliyeva H, Unal G, Tanalp TD. An overview of challenges to eradication of Helicobacter pylori infection and future prospects. Eur Rev Med Pharmacol Sci. 2017 May;21(9):2199-2219.
Hafeez, M., Qureshi, Z. A., Khattak, A. L., Saeed, F., Asghar, A., Azam, K., & Khan, M. A. (2021). Helicobacter Pylori Eradication Therapy: Still a Challenge. Cureus, 13(5), e14872.
Zongchao Liu, Hengmin Xu, Weicheng You, Kaifeng Pan, Wenqing Li. Helicobacter pylori eradication for primary prevention of gastric cancer: progresses and challenges. Journal of the National Cancer Center. 4 (4) 2024, Pages 299-310.
Argueta, Erick A. et al. How We Approach Difficult to Eradicate Helicobacter pylori. Gastroenterology, Volume 162, Issue 1, 32 – 37.
Articles that might interest you